 Your new post is loading...
 Your new post is loading...

|
Scooped by
nrip
|
Electronic health records are overloading outpatient docs with info in "disparate files and folders rather than presenting comprehensive, actionable data in a context that gives meaning," say researchers in a VA-funded study A primary care physician may care for 2,500 or more patients in a given year, and many of their patient encounters may last only 20 minutes – much of which is often spent at a computer with a back turned to the patient. It's become a truism by now that electronic health records are often viewed askance by primary care docs, many of whom see them as detrimental to the patient encounter. A new report from U.S. Department of Veterans Affairs, Regenstrief Institute and Indiana University details just how outpatient EHRs are often failing the physicians who use them. Why it matters
EHRs "are not rising to the challenges faced by primary care physicians because EHRs have not been designed or tailored to their specific needs," The report draws on eight years of close study of EHR use patterns to argue for wider acceptance of "human factor approach for the design or redesign of EHR user interfaces." many EHRs as currently configured make it too difficult for primary care docs to do their job in a streamlined and efficacious manner – requiring navigation through multiple screens and tabs to find basic information, increasing redundancy and decreasing efficiency. Something as simple as auto-save – a default capability for most online shopping, for instance – is missing from many EHR systems. Roots of the problem The study traces the roots of the challenge to the fact that many EHRs were initially designed for specialists and hospitals – without much attention to the specific needs of primary care physicians. For Primary care physicians, effective decision-making is grounded in perception and comprehension of a patient's dynamic situation." For example, they note, an outpatient doc's choice to stop a patient's use of a particular medication will usually be informed by trends in that patient's blood pressure or cholesterol numbers, or other medications taken over the course of a month – all holistic information with implications for the patient's future health trajectory, but data that isn't always readily seen on a single EHR screen. Technology needs to adapt to humans' needs, abilities, and limitations in healthcare delivery as it has in other domains. EHRs should be redesigned to improve situational awareness for busy primary care physicians and support their tasks including reviewing patient information, care coordination, and shared decision-making." read more at https://www.healthcareitnews.com/news/regenstrief-study-shows-ehrs-underperforming-primary-care

|
Scooped by
nrip
|
We developed and validated an accurate in-hospital mortality prediction score in a live EHR for automatic and continuous calculation using a novel model that improved upon SOFA. The COVID-19 pandemic created an emergent need for a novel, accurate, and location and context-sensitive EHR-computable tool to predict mortality in hospitalized patients with and without COVID-19. Because developing a new score can take years, a predictive model must rely on well-validated scores. In contrast, COVID-19 is a novel disease for which existing scores may be of limited but unknown predictive value. As such, a predictive framework relying on multiple previously validated scores that can incorporate new information but only keeps the new inputs that explicitly improve performance is required. Stacked generalization provides a solution. A stacked model is built upon one or more baseline model(s) (e.g. SOFA) and incorporates additional models only when they improve prediction. Materials and Methods We developed, verified, and deployed a stacked generalization model to predict mortality using data available in the EHR by combining five previously validated scores and additional novel variables reported to be associated with COVID-19-specific mortality. We verified the model with prospectively collected data from 12 hospitals in Colorado between March 2020 and July 2020. We compared the area under the receiver operator curve (AUROC) for the new model to the SOFA score and the Charlson Comorbidity Index. Results The prospective cohort included 27,296 encounters, of which 1,358 (5.0%) were positive for SARS-CoV-2, 4,494 (16.5%) required intensive care unit care, 1,480 (5.4%) required mechanical ventilation, and 717 (2.6%) ended in death. The Charlson Comorbidity Index and SOFA scores predicted mortality with an AUROC of 0.72 and 0.90, respectively. Our novel score predicted mortality with AUROC 0.94. In the subset of patients with COVID-19, the stacked model predicted mortality with AUROC 0.90, whereas SOFA had AUROC of 0.85. Discussion Stacked regression allows a flexible, updatable, live-implementable, ethically defensible predictive analytics tool for decision support that begins with validated models and includes only novel information that improves prediction. read the paper abstract at https://academic.oup.com/jamia/advance-article/doi/10.1093/jamia/ocab100/6273353 read the entire paper at https://academic.oup.com/jamia/advance-article-pdf/doi/10.1093/jamia/ocab100/37905236/ocab100.pdf

|
Scooped by
nrip
|
Boston Medical Center reduced the number of patients who received unnecessary diagnostic testing after implementing new recommendations into its electronic medical record (EMR) system. The study, published in the Joint Commission Journal on Quality and Patient Safety, looked at the effectiveness of implementing electronic health record (EHR)-based interventions to promote high-value care. The hospital saw significant decreases in pre-admission chest x-rays and labs ordered at routine times six months after the implementation. The proportion of patients that received pre-admission chest x-rays significantly decreased 3.1 percent; the proportion of labs ordered at routine times decreased 4 percent; and total lab utilization declined 1,009 orders per month. The proportion of postoperative patients who received appropriate pain and pneumonia prevention orders increased 20 percent, the results revealed. However, there was no significant difference in the estimated red blood cell transfusion utilization rate or number of non-ICU urinary catheter days following the implementation. While the interventions reduced diagnostic testing, they did not have a significant effect on clinical interventions. more at https://www.clinical-innovation.com/topics/ehr-emr/emr-solutions-decrease-unnecessary-lab-testing

|
Scooped by
nrip
|
Incorporating persuasive design concepts into primary care electronic health records (EHRs) increased same-day data entry by 10 percent per physician, demonstrating the potential for persuasive design to change data entry behavior, a study published in JMIR Human Factors revealed. Persuasive design is a way of developing technology to influence behavior by leveraging social processes. Healthcare stakeholders have primarily focused on using persuasive design in consumer-facing mobile apps to improve outcomes, but there are few examples of using persuasive design to influence clinician behavior. In primary care settings, providers often face barriers to entering data into EHRs in a timely manner. Data entry tasks often take a long time, and users may feel as if completing documentation is a lower priority than seeing patients or finishing other tasks. “Persuasive design is a viable approach for designing and encouraging behavior change and could support effective data capture in the field of medical informatics. There may be opportunities to continue improving this approach, and further work is required to perfect and test additional designs,” the team concluded. read the original unedited article at https://healthitanalytics.com/news/persuasive-ehr-workflow-design-increased-same-day-data-entry-by-10

|
Scooped by
nrip
|
Suki, the artificial intelligence (AI) voice assistant for healthcare professionals, launched in May to praise from health-tech innovators who hoped “Alexa for doctors” might slash electronic health record (EHR) documentation time.
If the company’s early numbers are any indication, that wish might come true.
Suki said recently that doctors who use the digital assistant have seen a 70 percent drop in time spent writing and filing medical notes. That figure is 10 percentage points better than the preliminary results of Suki’s pilot. The finding could prove powerful, as research has suggested that physicians burn almost two hours in the EHR for every hour of patient interaction. Suki has processed more than 12,000 patient encounters in the real world, handling 1,000 per week, according to the company. This steady stream of real-world data is poised to strengthen the technology’s machine-learning algorithm, which was trained on 250,000 patient encounters before it went live.
So far, Suki has integrated with three EHR systems. The company said that number is slated to rise.
Using voice commands, the technology pens a “clinically accurate” note that it then sends to a doctor’s EHR system.
Over the past several years, innovators across healthcare have advocated for a clinical voice assistant. But the challenges are many, from precise listening and documentation to satisfying cybersecurity concerns.
Although a clinical AI assistant might be far off for many providers and health systems, Suki and similar technologies could help solve a mounting problem in medicine: physician burnout.
Time spent in the EHR has been linked to physician burnout. On the conference circuit and in the opinion pages, doctor after doctor describes the stresses of medical note documentation — and how these demands eat up time and detract from care delivery.
Can Suki help improve workflows? It seems so. But can it go a step beyond and help physicians overcome burnout? Maybe. The answer to that question will depend on adoption rates and how Suki performs at scale.
Will Suki become a part of the clinic of tomorrow? Lets wait and see read the unedited story at https://www.hcanews.com/news/alexa-for-doctors-claims-70-percent-reduction-in-ehr-time

|
Scooped by
nrip
|
“Universal EHR” structures, in which every citizen’s electronic health record is connected to a single national system, are tied to higher trust in the healthcare system and higher value for patients, Unified electronic records have also prompted national governments to address issues of privacy and security, data integrity, and health information exchange that are left up to the private sector in other countries – with varying degrees of success. Half of the 16 countries included in the index have universal EHRs, while the other half have let a combination of free market forces and regulatory guidance dictate the course of health IT adoption. The eight countries with universal EHRs saw an average overall “Value Measure” of 47.29, the report says. The Value Measure is a combined score based on access to care, patient satisfaction, and an efficiency ratio score. Now, Healthcare providers in the United States generally don’t harbor very warm feelings for their electronic health records (EHRs). Despite efforts from vendors and regulators to improve the experience of interacting with these foundational health IT systems, dissatisfaction and frustration with usability issues and fragmented information are still causing users’ blood to boil. It may seem counterintuitive, therefore, to suggest that expanding the industry’s reliance on EHRs is actually the key to making EHR use less stressful and more useful – but that is exactly what the 2018 Future Health Index, commissioned by Philips, seems to indicate.

|
Scooped by
nrip
|
Microsoft says care coordination and secure messaging tools are coming to its Teams platform Microsoft is holding its Ignite conference this week, and the company teased a forthcoming care coordination tool that is in early stages of development – as well two secure messaging features it's creating as part of an effort to tailor Teams for specific industries. "As an example of how Teams can enable secure workflows for regulated industries, we're delivering a new care coordination solution, now available in private preview, that gives healthcare teams a secure hub for coordinating care across multiple patients," Ron Markezich, Corporate Vice President for Microsoft 365, wrote on the company's blog. "It provides for integration with electronic health record systems and enables care providers to communicate about patient care in real-time within Teams' secure platform.” Markezich said Microsoft is also releasing two new secure message capabilities for Teams: one for for image annotation and the other for priority notifications. While the image function is already generally available, the priority notifications feature is scheduled to be available for companies that use the commercial version of Teams by year's end. "These capabilities support HIPAA compliance and enable doctors, nurses, and other clinicians to communicate about patients while avoiding the privacy risks that arise when healthcare professionals use consumer chat apps," Markezich added. Microsoft said the new care coordination tools will integrate with EHR systems so clinicians and caregivers can communicate via the Teams platform. Considering that the average hospital has 16 different EMR vendors across all its affiliated practices, that integration won't be as easy as it might sound. That said, the tech is in "private preview" mode, so it's a bit early to tell what shape it will take by the time it reaches the open market. read the original story at https://www.healthcareitnews.com/news/microsoft-says-care-coordination-and-secure-messaging-tools-are-coming-its-teams-platform

|
Scooped by
nrip
|
Clinical documentation improvement (CDI) ensures that health services are accurately documented and helps healthcare coders and physicians work toward improved patient care while also streamlining productivity. When meaningful clinical data is captured, organizations can ensure improved quality reporting, clinician productivity, and even better clinical information delivered at the point of care. Phoenix Children’s Hospital recently opted for CDI at its outpatient clinics with Medicomp Systems. It’s important to help physicians make patient care faster, safer, and more efficient. Every single symptom, sign, medication, surgery, drug, operation procedure, almost a repository of more than 360,000 terms, they have structured and coded with every possible common coding schema, such as ICD-10,” he continued. Having 360,000 terms can be overwhelming, but they were built along disease patterns. If a physician entered that a patient had asthma, or tried to research asthma in the database, it went out to all related items that were related to asthma and it brought them together in a manner of an automatic template that was a quick, rapid initial draft. There is no magic formula with clinical documentation and finding an applicable system for an organization. “You cannot take shortcuts. You cannot not capture things that are critical and essential,”

|
Scooped by
nrip
|
The EHR interoperability challenge is what stands between a physician's ability to look up, extract, and track a patient's medical activities and records at medical sites other than their own. This could be at a laboratory where a patient's specialty blood work is being analyzed or they're having surgery on an inpatient or outpatient basis. When it comes to tracking these patients, it's literally as they move about in the sphere of the healthcare world. The interoperability challenge occurs because you need your EHR to talk to systems outside your practice. Solving this challenge means maintaining continuity of care for patients, minimizing or eliminating the duplicity of services, and helping physicians share patient information so they can gain insight from specialists that would complement their diagnoses. Many EHR companies aren't willing to share access to their systems unless a physician is part of their overall user base. If you work in a particular hospital or practice that has their product, these particular companies will share information with physicians. The problem is they won't work with peripheral players, or physicians who are unaffiliated with the hospital or practice where their EHR is installed. Why is it in the hospital's interest to provide access to patients via their EHR? Sharing access to patients via the hospital's EHR creates a win-win situation where the hospital can keep the patient in their system. these are excerpts from an interview David Wasserman, an advisor with the practice solutions and medical economics group at the Massachusetts Medical Society. read more at the original http://www.diagnosticimaging.com/ehr/solving-ehr-interoperability-challenge

|
Scooped by
nrip
|
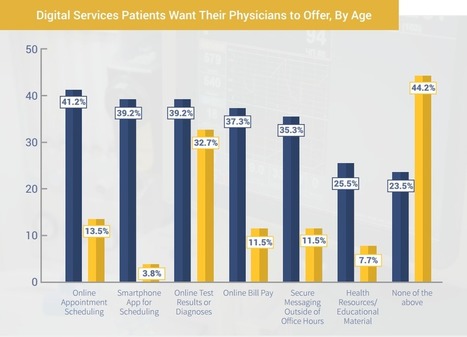
New patient engagement trends from TechnologyAdvice Research reveals digital engagement is a growing factor in how patients choose healthcare providers.
Quality of care has long been a primary factor in choosing a healthcare provider, but convenience and communication are also becoming key considerations for patients. Still, many physicians do not appear to be offering the digital engagement services that can meet those demands.
According to a new nationwide survey conducted by TechnologyAdvice Research, a majority of patients (60.8 percent) said digital services like online appointment scheduling and online bill pay are either “important” or “somewhat important” when choosing a physician. However, when asked what services their current physician provides, less than one-third of patients indicated they have access to either online bill pay, online appointment scheduling, or the ability to view test results and diagnoses online, which are the top three services that patients report wanting the most.
“Primary care physicians are reporting some of the highest rates of EHR adoption to comply with government regulations and to receive incentives from Meaningful Use, but a significantly lower number of patients claim to have access to these patient portal services,” said TechnologyAdvice Managing Editor Cameron Graham, who authored the survey. “The issue here may not be implementation of digital services, but instead a lack of patient awareness. If physicians are offering these in-demand digital services, a more proactive approach to promoting them is needed and could create an advantage in attracting and retaining patients.”
TAKEAWAYS
- If providers wish to gain an upper edge in attracting new patients (especially younger ones), and in retaining their existing patients, they should invest in a fully featured patient portal system. For many primary care physicians this should not be difficult. Most comprehensive EHRs include patient portal features, and dedicated patient portal vendors are making strides in integrating with third-party systems. In particular, prioritizing systems with intuitive online appointment scheduling, online bill pay functionality, and online test results could provide a significant draw for new patients.
- For practices that already have patient portal systems, they should dedicate resources to making sure their patient populations are informed of the existence of such services. They should also consider prominently featuring these services in their advertising and on their websites. When orienting new patients to their practice, providers need to have a plan for walking patients through the initial portal set-up requirements and making sure they understand the features available to them.
-For particularly tech-savvy practices, a dedicated smartphone app could help set them apart, and attract younger individuals.
more at http://hitconsultant.net/2015/01/16/should-physicians-tailor-patient-engagement-based-on-age/

|
Scooped by
nrip
|
Legislation that incorporates psychiatric care into the acute-care spectrum and extends EHR incentives to behavioral health facilities has been proposed for going on five years now.
A show of hands: Who believes depression or bipolar disorder have no impact on the severity and treatment of a patient’s diabetes and COPD? It’s an idea no practicing physician would support.
Yet time and again, we act as though mental illness and care can be kept separate from physical ailments.
Take Meaningful Use (MU), for example. The federal government believes healthcare must move into the digital age and is willing to pay hospitals to buy computer systems and electronic health records (EHRs).
But the financial rewards of demonstrated MU only extend to acute care hospitals and clinics, not psychiatric facilities, as though human health can be partitioned and compartmentalized.
While treating patients holistically has been accepted clinically for decades, some behavioral health advocates are turning up the pressure now to finally also bring behavioral health IT into the digital age.
more at http://hitconsultant.net/2015/01/20/why-behavioral-health-acutely-needs-ehrs/

|
Scooped by
nrip
|
Can we standardize and personalize healthcare at the same time? James Dias, CEO and Founder of Wellbe shares how we can do both to improve patient care.
Usually when personalization is mentioned in the world of healthcare thoughts jump to genetics and personalized medicine with custom cancer drugs and medical devices. However, there is another type of personalization that can be applied to healthcare, to make each patient feel like an individual, rather than just “one of the masses.”
The world of ecommerce discovered the value of personalized online experiences a decade ago and the additional revenue/branding/loyalty that can be generated from it. For example, the NikeiD website offers customers the ability to customize their own shoes. Who can forget the “Elf Yourself” campaign from Office Depot, where you could stick your friends’ and family’s faces on to happy dancing elves? With the new year upon us, fewer people are opting to buy regular old glossy calendars when a dozen photo sites will let you make a custom one from your personal photos.
Personalization is all around us, from the recommendation engines of Netflix and Amazon, to the custom radio stations you can create on Pandora. Smart programs have figured out what’s relevant to each of us and help filter the signal from the noise in today’s massive universe of information. As consumers, we engage and respond much more positively to these personalized experiences, which encourages loyalty and repeat business.
The psychology of personalization shows that engaging the customer in the process helps build a psychological and emotional attachment to their purchase. In addition, increasing customer participation boosts feelings of control and ensures satisfaction at the point of sale.
Similarly, by offering a personalized digital healthcare experience, we can increase patients’ ownership of their health and outcomes. Often it seems that patients feel they have no control over their outcomes, when actually the opposite is true. When they feel like active participants in their health journeys, it is more likely they will achieve the outcomes they desire, and they will feel like they got better value for their dollar.

|
Scooped by
nrip
|
Millennials and Baby Boomers alike want more from their EHR, especially access through portals.
Last year’s annual EHR survey from Xerox found patients desired more information on EHRs and thought their providers should give more EHR education. This year, Xerox reports their 2014 annual EHR survey finds patients desire access to their records through portals - and it’s not just younger patients who are looking for digital access.
Health Data Management reports about a third of patients said simple knowledge of portals was lacking. Of those who said they did not use portals, 35 percent did not even know a portal was available and 31 percent said their physician had never spoken to them about portals.
A second study by Technology Advice found 40 percent of patients don’t know if their provider offers an online portal, even though a third study showed simply taking to patients about portals increases their use.
|

|
Scooped by
nrip
|
Patient travel history can be crucial in evaluating evolving infectious disease events. Such information can be challenging to acquire in electronic health records, as it is often available only in unstructured text.
Objective: This study aims to assess the feasibility of annotating and automatically extracting travel history mentions from unstructured clinical documents in the Department of Veterans Affairs across disparate health care facilities and among millions of patients. Information about travel exposure augments existing surveillance applications for increased preparedness in responding quickly to public health threats.
Methods: Clinical documents related to arboviral disease were annotated following selection using a semiautomated bootstrapping process. Using annotated instances as training data, models were developed to extract from unstructured clinical text any mention of affirmed travel locations outside of the continental United States. Automated text processing models were evaluated, involving machine learning and neural language models for extraction accuracy.
Results: Among 4584 annotated instances, 2659 (58%) contained an affirmed mention of travel history, while 347 (7.6%) were negated. Interannotator agreement resulted in a document-level Cohen kappa of 0.776. Automated text processing accuracy (F1 85.6, 95% CI 82.5-87.9) and computational burden were acceptable such that the system can provide a rapid screen for public health events.
Conclusions: Automated extraction of patient travel history from clinical documents is feasible for enhanced passive surveillance public health systems.
Without such a system, it would usually be necessary to manually review charts to identify recent travel or lack of travel, use an electronic health record that enforces travel history documentation, or ignore this potential source of information altogether. The development of this tool was initially motivated by emergent arboviral diseases. More recently, this system was used in the early phases of response to COVID-19 in the United States, although its utility was limited to a relatively brief window due to the rapid domestic spread of the virus. Such systems may aid future efforts to prevent and contain the spread of infectious diseases. read the study at https://publichealth.jmir.org/2021/3/e26719

|
Scooped by
nrip
|
Clinical decision support (CDS) alerts may not seem significant on the surface, but these alerts have the potential to save patient lives. CDS alerts permit clinicians to access real-time patient data, ideally resulting in enhanced patient safety and medication accuracy. CDS alerts can also notify clinicians about potential patient warnings to prevent errors and additional adverse drug events from occurring. While EHRs are directly associated with clinician burnout, CDS tools aim to aid clinicians. CDS “provides clinicians, staff, patients or other individuals with knowledge and person-specific information, intelligently filtered or presented at appropriate times, to enhance health and health care.” The benefits they offer include: Identifying Adverse Drug Events Promoting Patient Safety Improving Patient Awareness, Improve Provider-Patient Communication Where they have been found to be ineffective in current times - Alert Fatigue and Low-Value Alerts Failure to Detect Medication Errors Commercial Influence CDS alerts are an imperfect EHR tool with several pros and cons. But increased stakeholder research could minimize the number of negatives and expand the number of positives. Read the whole article at https://ehrintelligence.com/news/the-pros-and-cons-of-ehr-clinical-decision-support-alerts

|
Scooped by
nrip
|
In a study published in the AMA Journal of Ethics, researchers explored the role of social and behavioral data in precision medicine research. Electronic health records (EHRs) can offer information on social and behavioral data, which can aid research investigating genetic and social factors across health disparities; for example, factors such as substance use and eating habits inform some of the risk associated with preventable premature deaths in the United States. Brittany Hollister, PhD, and Vence L. Bonham, JD, from the National Human Genome Research Institute at the National Institutes of Health, discussed potential biases in collecting, using, and interpreting EHR-based data in precision medicine research. Current collection of behavioral and social data by precision medicine researchers is increasingly done using EHR data, as opposed to self-report methods such as surveys. However, extraction and use of EHR data poses challenges of inconsistencies or inaccuracies. Another challenge is determining what data are included or excluded from EHRs, and the consequences of using data collected through biased methodologies. The National Academy of Medicine addressed some of this in recommendations for the systematic capture of behavioral and social measures.2 They recommended intentional collection of structured social environment data, as well as the development of a plan by the National Institutes of Health to include social and behavioral data in EHRs. The current inconsistencies in collecting social and behavioral data pose difficulties to use in precision medicine research, but with improved collection methods these difficulties could be amended. more at https://www.medicalbag.com/ethics/precision-medicine-research-ehr-data/article/808747/

|
Scooped by
nrip
|
A new project launched by Penn Medicine last week will take on the monumental task of EHR usability. Impatient with the current progress of electronic health records (EHRs), one of the nation’s foremost academic medical centers is taking matters into its own hands. Last week, Penn Medicine—which operates as the health system under the University of Pennsylvania—launched a new initiative aimed at transforming EHRs into “more streamlined, interactive, smarter tools.” That effort will focus primarily on what David Asch, M.D., the executive director of the Penn Medicine Center for Health Care Innovation, calls “the middle space” between EHRs and clinical productivity. “It’s about the creation of some middleware that takes the EHR products created by large companies and creates interfaces that are better,” he told FierceHealthcare. “It might ultimately be absorbed by those [EHR] companies, but I don’t think we can wait. I don’t think we should force clinicians to move to the EHR when we can be a part of the solution to help bring the EHR to them.” Part of Penn Medicine’s effort is a focus on using EHRs not just as an administrative or documentation tool, but also pushing it into the care delivery arena. That involves shaking up the traditional health system approach that says clinicians simply need more education to unlock the unused functionality of EHRs. The notion that clinicians need help becoming the “master of the EHR” often rubs them the wrong way, Asch says. more at https://www.fiercehealthcare.com/tech/penn-medicine-s-new-transformation-project-middle-space-ehrs-and-clinicians

|
Scooped by
nrip
|
A study to correlate EHR Communication with patient outcomes for diabetes patients reported that "EHR team communication flow patterns may be an important avenue to explore in raising quality of care and lowering costs for patients with diabetes in primary care." The study found that Primary care teams whose EHR communication reached more team members indirectly (ie, via message forwarding) had worse outcomes and higher medical costs for their patients with diabetes. The study was carried out to determine how changes in electronic health record (EHR) communication patterns in primary care teams relate to quality of care and costs for patients with diabetes.
The Study Design: EHR-extracted longitudinal observational study.
A total of 83 health professionals in 19 care teams at 4 primary care clinics associated with a large Midwestern university participated in the study. Counts of messages routed between any 2 team members in the EHR in the past 18 months were extracted. Flow-betweenness, defined as the proportion of information passed indirectly within the team, was calculated. The analysis related changes in team flow-betweenness to changes in emergency department visits, hospital stays, and associated medical costs for the teams’ patients with diabetes, while adjusting for team face-to-face communication, patient-level covariates, comorbidities, team size, and clinic fixed effects.
Results: Patient hospital visits increased by 13% (standard error [SE] = 6%) for every increase of 1 percentage point in team EHR message forwarding (ie, higher team flow-betweenness). Medical costs increased by $223 (SE = $105) per patient with diabetes in the past 6 months for every increase of 1 percentage point in team flow-betweenness.
Conclusions: Primary care teams whose EHR communication reached more team members indirectly (ie, via message forwarding) had worse outcomes and higher medical costs for their patients with diabetes. EHR team communication flow patterns may be an important avenue to explore in raising quality of care and lowering costs for patients with diabetes in primary care. read the whole study details at https://www.ajmc.com/journals/issue/2018/2018-vol24-n10/putting-the-pieces-together-ehr-communication-and-diabetes-patient-outcomes

|
Scooped by
nrip
|
Scribes have the potential to address several causes of physician burnout at primary care practices High-quality scribes generate high-level gains in primary care practices. That's the conclusion of recent research published in JAMA Internal Medicine, which found scribes decreased physician EHR documentation burden, boosted work efficiency, and improved patient visit interactions. Scribes can have a significant impact on a prominent factor for physician burnout, the researchers wrote. "Emerging evidence indicates that EHRs, as currently implemented, increase clerical workload and physician stress and interfere with direct physician-patient interaction, thereby diminishing professional satisfaction and contributing to professional burnout," the researchers wrote more at https://www.healthleadersmedia.com/clinical-care/scribes-slash-physician-ehr-burden-boost-efficiency-improve-patient-visits

|
Scooped by
nrip
|
Olive automates repetitive tasks and can match patients across databases at different hospitals When Sean Lane, a former NSA operative who served five tours of duty in Afghanistan and Iraq, first entered into the health care-AI arena, he was overwhelmed with data silos, systems that don’t speak to each other, and many, many portals and screens. “I was not going to create another screen,” Lane told a packed room on Monday at ApplySci’s annual health technology conference at the MIT Media Lab in Cambridge, Mass. Instead, Lane and a team taught an AI system to use software that already exists in health care just like a human would use it. They named it Olive. “Olive loves all that crappy software that health care already has,” said Lane. “Olive can look at any software program, any application for the first time she’s ever seen it, and understand how to use it.” For example, Olive navigates electronic medical records, logs into hospital portals, creates reports, files insurance claims, and more. Olive does so thanks to three key traits. First, using computer vision and Robotic Process Automation, or RPA, the program can interact with any software interface just as a human would, opening browsers and typing. Second, machine learning enables Olive to make decisions the way human health care workers do. The team trained Olive with historical data on how health care workers perform digital tasks, such as how to file an insurance eligibility check for a patient seeking to undergo a procedure. Finally, Olive relies on a unique skill that Lane developed based on his work at the NSA identifying criminals across disparate government sources—the ability to match identities across databases. Just as NSA software can determine if a terrorist in the CIA database is the same as in the Homeland Security database, so Olive matches a patient across disparate databases and software, such as multiple electronic health care record programs. Read the full article at https://spectrum.ieee.org/the-human-os/computing/software/this-healthcare-ai-loves-crappy-software

|
Scooped by
nrip
|
At the World Medical Innovation Forum this week, participants were polled with a loaded question: “Do you think healthcare will become better or worse from the use of AI?” Across the respondents, 98 percent said it would be either “Better” or “Much Better” and not a single one thought it would become “Much Worse.” This is an interesting statistic, and the results were not entirely surprising, especially given that artificial intelligence was the theme for the meeting. This continual stream of adoption of new technologies in both clinical and post clinical settings is remarkable. Today, healthcare is a technology operation. As a case in point, outside of the array of MDs and medical professionals presenting at the forum, there was clearly a strong, advanced technology thread weaved throughout the conversations of the traditional topics of pathology, radiology, bioinformatics, electronic medical records (EMR), and standard healthcare provider issues. As an example, a panel of senior technology experts from Microsoft, Cisco Systems, Dell EMC, Qualcomm, and Google joined research and information officers from Partners Healthcare and Massachusetts General Hospital to discuss the challenges in what they called “Data Engineering in Healthcare: Liberating Value.” That is a serious title for a panel. Data portability was clearly a key topic, as was security and the public cloud. The underlying issue with the cloud is that the EMR was never really designed to be portable. Health records existed with institutional walls, and were not originally intended for real time care, but more as a means of tracking costs and transactions as the patient traveled through the various systems. As the EMR has not only become more feature rich, the ability to mine that data inside of them with ML and AI methods is clearly at the forefront of everyone’s mind right now. There was discussion of episodic systems wrapped in policy and technology – this really isn’t quite how we can gain the maximum knowledge from the healthcare version of a Digital Me. A digital object containing all of our many and varied health related attributes. The challenges of discussing how to best build a “marketplace” and healthcare data exchanges and how to integrate “data marts” with existing EMR systems was obvious.

|
Scooped by
nrip
|
As patients become familiar with medical records and clinical notes, they consider new opportunities and risks. Some say they have become more careful about what information they share with clinicians, and some ask for more control over access to their information.
Providers are experimenting with strategies that help patients protect their privacy with regard to mental health, sexual function, suspected abuse, or other sensitive topics. And though family caregivers may find that reading notes improves their understanding of care plans and reduces stress, it's a complex task to establish separate proxy access based on patients' preferences about who gets to see what. As transparent practice evolves, it's impossible to predict how much patients may stray from long-standing conventions. Portals afford patients secure access to their information, and doctor–patient confidentiality remains undisturbed.
But patients' attitudes toward privacy may change as online access allows them to share documents, including notes. A third of patients in the OpenNotes study expressed concern about privacy, but more than one in five shared a note with others who could clarify meanings, offer clinical insights or second opinions, or — for those participating in the patient's care — improve their own knowledge. Indeed, some patients may choose to post their providers' progress notes on Facebook, Twitter, medical forums, and other social media, potentially exposing clinicians to public scrutiny and crowd-fueled praise or criticism.

|
Scooped by
nrip
|
A new report finds that while nearly all physicians have a smartphone, few said they would use their personal phone to access electronic health records. Meanwhile, 70% of physicians said hospital IT organizations are not making adequate investments in physician mobile computing and communication.
The report found that doctors prefer to use consumer text messaging for clinical communication over secure messaging applications because it is simpler to do so.
Eighty-three percent of respondents expressed frustration over using an EHR system for clinical communication due to:
- Inadequate messaging capabilities;
- Limited usability; and
- Poor interoperability
However, while 96% of physicians said they use smartphones, only 10% of those who do so said they would use them to access EHRs.
Meanwhile, 70% of respondents said they "believe that hospital IT organizations ... are making inadequate investments to address physician mobile computing and communication requirements at point of care."
more at http://www.ihealthbeat.org/articles/2015/1/15/report-few-doctors-use-personal-smartphones-for-ehr-access

|
Scooped by
nrip
|
Government health IT leaders say electronic health record systems can expand information sharing and help public health responders fight the spread Ebola and future viruses.
While the United States avoided a public health crisis from the Ebola virus, the possibility of an epidemic at home got government health IT leaders thinking about how electronic health records might be used to expand information sharing and help public health responders fight the spread of Ebola and future viruses.
There are significant hurdles to clear before the EHRs used in clinical care will be able to really help state, local and federal health officials track and respond to fast-moving outbreaks in real time, according to those at recent Health IT Policy Committee meeting on the potential for using EHRs to fight epidemics.
The problem of interoperability and data transfer between EHR systems, medical laboratories and public health databases is one big issue. More broadly, there is a lack of what experts call "bidirectionality" between health records, preventing health officials – either for technical or privacy reasons – from accessing individual patient records.
Ultimately, broader use of EHRs to detect and respond to epidemics will require changes in technology. The passive surveillance of patient EHRs using analytic tools could give greater velocity to detecting not just viral disease outbreaks, but environmental risks, contaminated food and medicine as well as other large-scale health problems that are clustered geographically or in certain demographic groups.
That’s not to say epidemiology is lacking in high-tech approaches. New York City, for example, was able to use cell phone location information and subway fare card data to conduct contact tracing on individuals that may have come into contact with the Ebola virus while traveling. However, aggregating that information, and making it available at scale through an EHR platform, appears to be a long way off.

|
Scooped by
nrip
|
With the wearables and health apps markets booming, where do doctors stand in terms of actually making use of the information?
So you are being proactive about your health by purchasing wearable devices and apps, but how helpful is it really if your doctor isn’t up to speed with the technology or able to interpret the data?
Dr. Paul Abramson, a primary care doctor in San Francisco told NPR that as much as these new devices are promoting good health generally, it’s not necessarily practical for doctors to interpret all of the data. “Going through it and trying to analyze and extract meaning from it was not really feasible,” he says. “I get information from watching people’s body language, tics and tone of voice. Subtleties you just can’t get from a Fitbit or some kind of health app.” Part of the issue is that FitBits and Apple Watches aren’t regulated by the FDA – they are considered “low-risk devices” and don’t require approval because they aren’t used for diagnosis or treatment. For that reason, it’s challenging for doctors to treat the data like valid information.
|



 Your new post is loading...
Your new post is loading...































Se le ofrece medicación sin receta, Farmacia España. – una de las farmacias más confiables de España, con más de 20 años de experiencia dispensando medicamentos de calidad
https://drogaspoderosas.com/producto/comprar-adderall-xr/
https://drogaspoderosas.com/producto/comprar-adipex-en-linea/
https://drogaspoderosas.com/producto/comprar-ambien-en-linea/
https://drogaspoderosas.com/producto/comprar-ativan/
https://drogaspoderosas.com/producto/comprar-blue-xanax/
https://drogaspoderosas.com/producto/comprar-botox-en-linea/
https://drogaspoderosas.com/producto/comprar-demerol-50mg-ml/
https://drogaspoderosas.com/producto/comprar-diazepam-en-linea/
https://drogaspoderosas.com/producto/comprar-dilaudid-8mg/
https://drogaspoderosas.com/producto/comprar-efedrina-hcl-30mg/
https://drogaspoderosas.com/producto/comprar-endocet-en-linea/
https://drogaspoderosas.com/producto/comprar-green-xanax/
https://drogaspoderosas.com/producto/comprar-hidrocodona-en-linea/
https://drogaspoderosas.com/producto/comprar-metadona-10mg/
https://drogaspoderosas.com/producto/comprar-morfina-15mg/
https://drogaspoderosas.com/producto/comprar-opana-en-linea/
https://drogaspoderosas.com/producto/comprar-stilnox-en-linea/
https://drogaspoderosas.com/producto/comprar-oxicodona-en-linea/
https://drogaspoderosas.com/producto/comprar-oxycontin-en-linea/
https://drogaspoderosas.com/producto/comprar-percocet-10mg-325mg/
https://drogaspoderosas.com/producto/comprar-rohipnol-2mg/
https://drogaspoderosas.com/producto/comprar-stilnox-en-linea/
https://drogaspoderosas.com/producto/comprar-suboxone-8mg/
https://drogaspoderosas.com/producto/comprar-subutex-8mg/
https://drogaspoderosas.com/producto/comprar-tableta-demerol/
https://drogaspoderosas.com/producto/comprar-vicodin-en-linea/
https://drogaspoderosas.com/producto/comprar-vyvanse-en-linea/
https://drogaspoderosas.com/producto/comprar-xanax-2mg/
https://drogaspoderosas.com/producto/compre-ritalin-en-linea/
https://drogaspoderosas.com/producto/parches-de-fentanilo/